How Ribbon Health and Databricks Unlock Better Patient Care

This blog post was written in collaboration with Eric Schwartz, Director of Partnerships at Ribbon Health, and David Kulwin, Director, Databricks Marketplace.
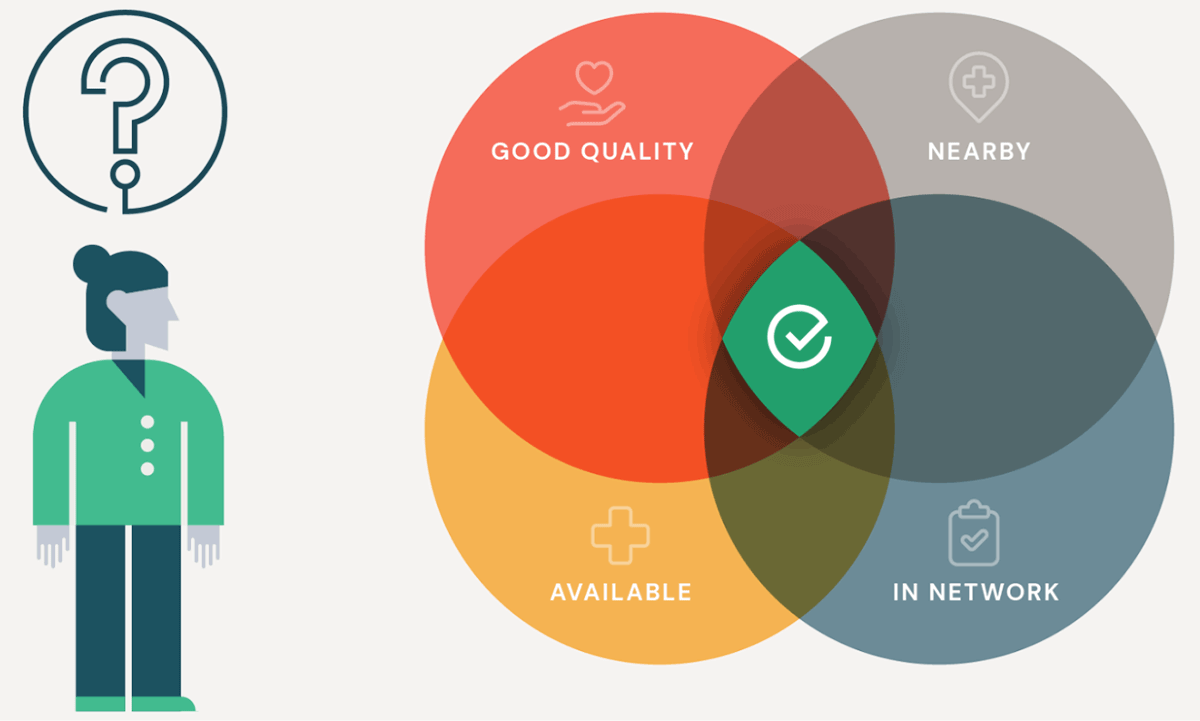
Ensuring individuals have access to both affordable and high-quality healthcare shouldn't be difficult. But there are formidable challenges embedded in our industry that unfortunately block patients from accessing care that fits their needs from a trusted and affordable provider. Connecting these dots between members, healthcare providers, and health plans involves intricate processes that can indeed be complex, time-consuming, and costly. A 2023 survey conducted by the Kaiser Family Foundation found that in the last year, 1 in 4 (26%) of insured adults were not able to find availability with a needed doctor covered by their insurance.
The core of this issue revolves around provider data. With hundreds of thousands of healthcare decisions made every year, this data must be timely, accurate, and accessible.
The opposite is true. Oftentimes, provider websites display outdated data such as old addresses and phone numbers. Even large organizations like health plans and provider systems are stricken with data issues that impact the quality of care:
- Roughly 50% of all provider entries have at least one inaccuracy: creating a single source of truth for provider data is a major challenge given that it is fragmented across 1,000+ data sources from disconnected systems. As a result, around half of provider directory data is inaccurate. This drains technical and operational resources, introduces compliance and financial risk, and creates barriers to people getting the care they need, negatively impacting member experience.
- 81% of provider data entries in the top 5 national health plans have inconsistencies: inaccurate provider directories can lead to surprise billing, access to care barriers, and network adequacy estimate challenges and misrepresentation. The core of the issue is the financial strain that directory reporting places on providers ($2.75 billion) and the lack of a standard for payers, which creates roadblocks to a centralized directory.
- $2.1 billion is spent annually on maintaining provider databases: this exorbitant cost is due to the lack of authoritative and reliable sources. As a result, the industry is forced to use a costly, piecemeal approach to acquiring and maintaining provider data.
As Dr. Kelly Kyanko Susan Busch wrote in The Hill in September of 2020, "The consequences of outdated directories can be more significant than just wasted hours on the phone and frustration. In addition to causing delays in care or even lack of care, outdated directories may result in surprise bills or unintentional care from an out-of-network provider."
The Ribbon Health story: When healthcare challenges get personal
Years ago, when our CEO Nate Maslak's mother started to experience joint pain, he saw firsthand how difficult it was to navigate the health system to find the right specialist that was near where his mother lived, was covered by her insurance, and had availability to see her soon. Nate was well-versed in the healthcare industry and jumped in to help his mother book an appointment - but she ended up at a back pain doctor, rather than a joint pain specialist. She was incorrectly referred to countless more providers, spending hundreds on visit fees, tests, and imaging each time.
Motivated by this experience, Nate and his co-founder, Nate Fox, launched HealthWiz as a care navigation company. Soon they realized that it was more than just a care navigation problem - this was a data challenge deeply rooted within the fabric of the healthcare ecosystem and those that suffered most were the patients.
They relaunched as Ribbon Health to partner with health plans, care navigators, primary care companies, and other organizations to solve the problem of fragmented and inaccurate provider data — in an effort to create a healthier future. Ribbon provides access to comprehensive provider information, including NPIs, practice locations, contact information, specialties, location types, relative cost and experience, areas of focus, and accepted insurance. The information is derived and maintained from thousands of data sources, billions of claims, advanced machine learning models, and human-in-the-loop model validation.
Customers typically use the Ribbon Health provider platform to power cost-effective, high-quality care navigation, improve member satisfaction, and conduct competitive network and gap analysis. Ribbon also offers provider data management services to help health plans more efficiently ingest, aggregate, cleanse, score, and maintain disparate provider data sources, including provider rosters delivered via email, data from legacy systems, and custom metadata.
The ROI of Ribbon Health for health plans & care navigators
Health plans need a comprehensive and reliable way to manage, assess, and maintain the accuracy of their provider data. This is critical for removing the operational burden of ensuring provider directories are an up-to-date truth set that enable care navigators and patients to quickly find a provider who is convenient, high quality, and with the expertise and the specific conditions they need help with. Traditionally, health plans have managed this on their own on legacy systems, often with extremely time-consuming and costly business rules associated with how they manage updates to their provider data. By leveraging the scalability and ease of use of the Databricks platform, Ribbon has been able to accelerate the pace of innovation with advanced, ML-powered data management capabilities for its customers.
By automating and scaling provider data management processes, Ribbon is helping both large health plans and upstart innovators in the healthcare space to increase member satisfaction, while significantly reducing care costs, by directing patients to the right provider the first time. With one payer-provider customer, Ribbon has helped decrease the customer's total medical expenses by 18%, resulting in more available doctors and better overall care. At another payer customer, Ribbon's technology to automate and scale data intake processes helps to achieve ~95% time-savings for provider admin.
How the Lakehouse helps Ribbon Health match patients with the right doctors
Putting ourselves in the shoes of our customers (health plans, health-tech companies, primary and specialty care groups), we needed to develop a solution that would help them improve patient care and innovate faster while reducing operational and financial overhead. While we looked at many data warehouses and data lake solutions, in the end, we decided to go with an architecture built on the Databricks Lakehouse. The Lakehouse makes it easy to create a single source of truth with full data governance and lineage which can then be used for all downstream use cases. This is critical as our goal isn't to just create a unified view of all this data, but also to create data solutions that are easy to slide into patient-facing and backend systems.
Below is an illustration of a common data workflow powered by Ribbon Health and Databricks Lakehouse:
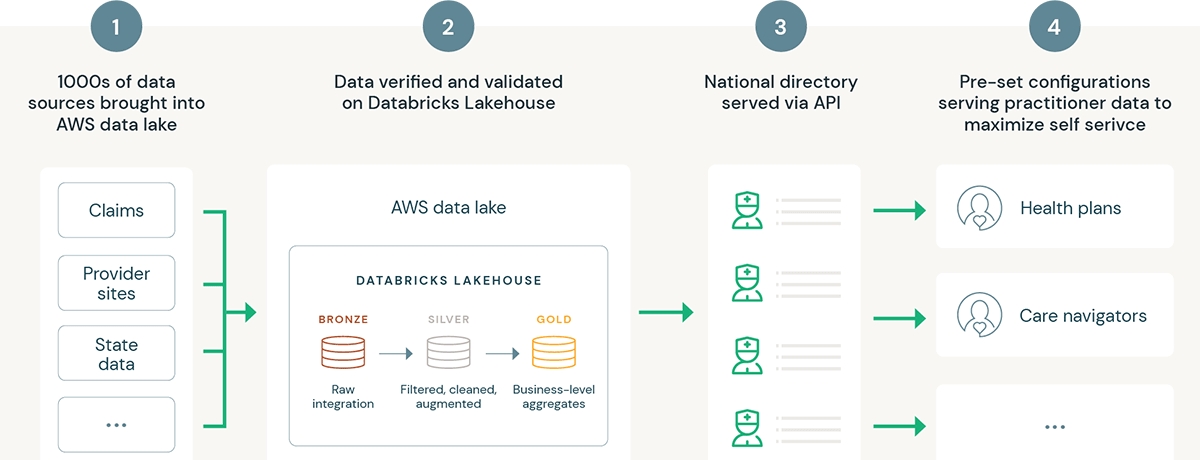
First, we bring in thousands of data sources like claims, provider/practice sites, state licensing, and more as raw data into our AWS data lake. This data is then fed to various ML models that clean and validate the data within our medallion architecture managed on the Databricks Lakehouse and Delta Lake. First data comes in as raw (bronze) and is normalized, validated, and processed in subsequent steps while maintaining full lineage.
The output is a national "Ribbon Foundation" directory, surfaced through an API, that makes it easy to serve backend and customer-facing systems with comprehensive, reliable provider searches and directory data.
For our Provider Data Management customers, Ribbon can integrate raw provider rosters in all of the forms they come in (Excel, email, pdf, etc.), leverage the Foundation directory as the source of truth to cleanse and score the data from customer-provided rosters, and then aggregate this information into a constantly updating directory that blends the best of the data sources - customer-specific data and provider networks plus Ribbon's comprehensive Foundation directory to enrich the directory with missing or incorrect data.
We can also work with customers to configure rules and best practices for data deconfliction and enrichment to mirror existing processes and streamline end-user workflows.
Full Ribbon provider, location directories now available with instant delivery on the Databricks Marketplace
We are happy to announce that we are one of the earliest partners represented in the Databricks Marketplace, an open marketplace for exchanging data products such as datasets, notebooks, dashboards, and machine learning models. You can now find Ribbon Health's Provider Directory & Location Directory on the Databricks Marketplace so health plans and care providers/navigators can start using this data today.
The data includes NPIs, practice locations, contact information with confidence scores, specialties, location types, relative cost and experience, areas of focus, and accepted insurance. The dataset also has broad coverage, including 99.9% of providers, 1.7M unique service locations, and insurance coverage for 90.1% of lives covered across all lines of business and payers. The data is continuously checked and cross-checked to ensure the most up-to-date information is shown.
With these data sets, organizations can now more efficiently manage, customize, and maintain their own provider data. Our customers can also increase the quality and comprehensiveness of their provider data by incorporating new data sources and scoring data accurately at scale, including provider rosters delivered via email, data from legacy systems, and custom metadata to help power provider search workflows via our Provider Directory Management offerings
Ribbon also offers its Provider Data Management offering, powered by Databricks, as a service to end-customers, including leveraging Delta Sharing and the full Databricks suite of capabilities to integrate data from existing customer data sources.
By leveraging Ribbon's capabilities through Databricks, customers can save significant time and cost with streamlined data flows, automate and scale data intake processes, and improve "Find Care" experiences to drive member satisfaction and retention.
To get started, check out Ribbon's provider data platform via the Databricks marketplace for more information.
Never miss a Databricks post
What's next?
Healthcare & Life Sciences
November 14, 2024/2 min read
Providence Health: Scaling ML/AI Projects with Databricks Mosaic AI
Product
November 27, 2024/6 min read